Congenital myasthenic syndromes
Congenital myasthenic syndromes (CMS) are rare inherited neuromuscular disorders characterized by fatigable weakness of skeletal muscle owing to compromised function of the neuromuscular junction (NMJ). The first identified mutations were in genes encoding subunits of the acetylcholine receptor, and these remain the most common subtypes of CMS worldwide. With the advent of next-generation sequencing, the number of genetic defects reported as causative of a CMS phenotype has increased dramatically, with over 30 genes now implicated. However, between 20 and 40% of patients with CMS remain without a molecular diagnosis after exome sequencing, and part of our research focuses on gene discovery to solve these remaining unsolved cases through the latest genome sequencing and multi-omics approaches.
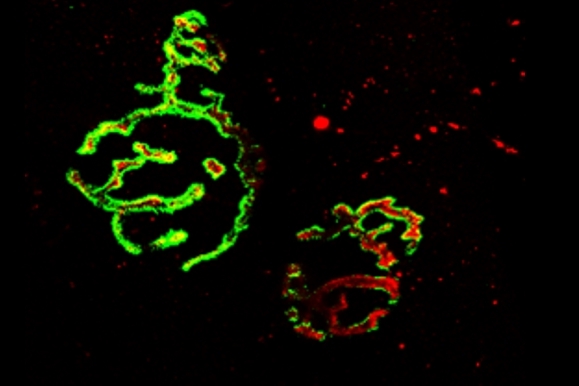
In many cases the pathomechanisms behind the disease are still not well understood, and our lab generates and works with cell, zebrafish and mouse models of various CMS subtypes in order to investigate the disease processes and look for therapeutic targets and disease modifiers.
Treatments for congenital myasthenia
Unlike the majority of neuromuscular disorders, congenital myasthenic syndromes are frequently treatable with common drugs that can significantly alleviate the severity of symptoms and restore some functional ability. Treatment varies by subtype, and treatment strategies are broadly dependent on whether it is beneficial to increase the amount of acetylcholine available in the synaptic cleft (for which commonly administered therapies include AChE inhibitors such as pyridostigmine, which inhibits acetylcholine breakdown, and the potassium-channel blocker 3,4-diaminopyridine, which increases the quantal release of acetylcholine) or to shorten the duration of synaptic current in slow-channel syndromes by reducing the channel-open time (for which the open-channel blockers fluoxetine and quinidine may be used). β2 adrenergic receptor agonists such as ephedrine and salbutamol (albuterol) are also widely prescribed for CMS. The mechanism of the therapeutic effect of β2 adrenergic receptor agonists in CMS is not understood, and our lab is investigating the mode of action of these drugs in specific CMS subtypes with the aim of exploring potential modifications to improve efficacy and better target treatment.
In collaboration with colleagues from the European Solve-RD project, we are working to develop a “treatabolome” for CMS – a database of treatable variants that can be incorporated into genetic databases and analysis systems in order to flag up to the treating clinician or geneticist that a potential treatment is available. The hope is that this will increase the speed with which individuals with CMS receive the correct treatment.
Read an article about the different CMS types and the way incorporating them into classification systems helps computer accessibility.
In collaboration with colleagues in Germany, we are currently working on the elucidation of the NMJ proteome and the establishment of a tailored assay enabling the robust quantification of NMJ-related proteins in various mouse models of this group of diseases.